Breast Cancer Detection & Diagnosis
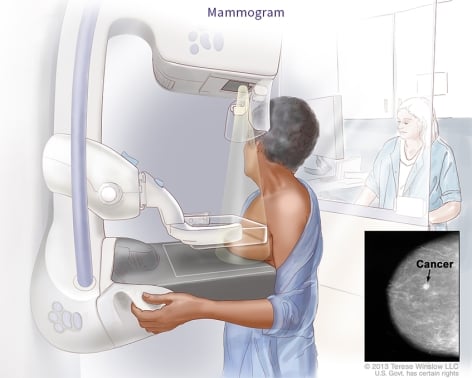
Breast cancer often shows no symptoms, which is why regular breast cancer screening is crucial. Although a hard lump in the breast is one of the symptoms, breast cancer can be found much sooner, when it’s easier to treat, through a mammogram.
Mammography is the most effective way to detect breast cancer early. Early detection increases the likelihood of successful treatment. If a routine mammogram detects an abnormal area, a diagnostic mammogram and possibly a breast ultrasound will be performed to investigate further and determine if cancer is present. It’s also important to note that cancer is not always diagnosed when an abnormal area is found in the breast. The only way to know for sure is through further testing.
The breast cancer specialists at Virginia Oncology Associates have created this video guide on breast cancer screening.
Mammogram: The Standard for Early Breast Cancer Detection
Breast cancer screening is guided by risk level and ranges from average to high. To help determine your risk level, the American College of Radiology (ACR) and the Society of Breast Imaging (SBI) recommend all women speak with their physician around the age of 25 to determine their breast cancer risk and the appropriate age to begin screening.
Regular screening mammograms to detect breast cancer early should become a part of every woman’s regular healthcare routine once you’ve reached the age for screening.
Recommendations for screening are based on whether you are considered average or high-risk.
Determining if You Are at High Risk for Breast Cancer
Women with a higher risk of developing breast cancer only need to meet one of the following criteria:
- Having a mother, sister, or daughter, considered a first-degree relative, who has had breast cancer. Risk also increases if you have multiple family members on either your mother or father's side of the family who have had breast or ovarian cancer.
- Having dense breast tissue
- Inherited BRCA1 or BRCA2 gene mutations
- Exposure to chest radiation before age 30
- Other high-risk situations determined by your provider
Your doctor may request you fill out a breast cancer risk questionnaire to gauge your lifetime risk. If your lifetime risk is found to be 20% or higher, you may be suggested to follow a high-risk screening process. This process might include MRI surveillance and annual mammograms starting as early as 25 years old, depending on your risk type.
Discussing your breast cancer risk with your physician can help you determine the right time to start breast cancer screenings.
Related reading: 5 Ways to Reduce Your Breast and Ovarian Cancer Risk When You're BRCA-Positive
Breast Cancer Screening for Women of Average Risk
The American Cancer Society (ACS) states women considered average risk for developing breast cancer are those who have no personal history of breast cancer, no family history of breast cancer, or no known genetic mutation (BRCA-1 or BRCA-2). For this category, the ACS recommends the following breast cancer screening program:
- Women age 40-44*: optional annual mammograms
- Women age 45-54: annual mammograms
- Women 55 and older: if in good health, annual or biennial (every other year) mammograms
*As of April 30, 2024, The United States Preventive Services Task Force (USPSTF) recommends all women start screening mammograms at age 40. For specific recommendations, talk to your doctor.
Screening should continue as long as a woman is in good health and is expected to live at least ten more years.
If you have never had a mammogram, read more about what to expect at your first mammogram.
What Happens if Your Mammogram Shows an Abnormal Area?
If the mammogram shows an abnormal area in the breast, your doctor may order clearer, more detailed images of that area. Doctors use diagnostic mammograms to learn more about unusual breast changes, such as a lump, pain, thickening, nipple discharge, or change in breast size or shape. Diagnostic mammograms may focus on a specific area of the breast. They may involve special techniques and more views than screening mammograms.
Doctors may also use other diagnostic imaging methods to gather more information about the lump or other unusual areas.
- Breast Ultrasound: A woman with a lump or other breast change may have an ultrasound test. An ultrasound device sends out sound waves that people can’t hear. The sound waves bounce off breast tissue. A computer uses the echoes to create a picture. The picture may show whether a lump is solid, filled with fluid (a cyst), or a mixture of both. The radiologist will determine whether a biopsy or further imaging is needed.
- Breast MRI: MRI uses a powerful magnet linked to a computer. It makes detailed pictures of breast tissue. These pictures can show the difference between normal and diseased tissue.
If Breast Cancer is Suspected, a Breast Biopsy is Next
A biopsy is the removal of tissue in the breast to see if cancer is present. A biopsy is the only way to tell for sure if there are cancerous cells.
Your doctor may refer you to a surgeon or breast disease specialist for a biopsy. The surgeon or doctor will remove fluid or tissue from your breast in one of several ways:
- Fine-needle aspiration biopsy: Your doctor uses a thin needle to remove cells or fluid from a breast lump.
- Core biopsy: Your doctor uses a wide needle to remove a sample of breast tissue.
- Skin biopsy: If there are skin changes on your breast, your doctor may take a small sample of skin.
- Surgical biopsy: Your surgeon removes a sample of tissue.
- An incisional biopsy takes a part of the lump or abnormal area.
- An excisional biopsy takes the entire lump or abnormal area.
A pathologist will check the tissue or fluid removed from your breast for cancer cells. If cancer cells are found, the pathologist will also describe other characteristics of the cancer, including the type of breast cancer and hormone status.
Note that a biopsy is not an automatic cancer diagnosis. Biopsy results can come back with information showing a non-cancerous condition is present. Typically, biopsy results take a few days to come back.
Lab Tests with Breast Tissue
If you are diagnosed with breast cancer, additional tests are performed on the breast tissue to help guide your treatment plan. These tests may include:
- Hormone receptor tests: Some breast tumors need hormones to grow. These tumors have receptors for the hormones estrogen, progesterone, or both. If the hormone receptor tests show that the breast tumor has these receptors, then hormone therapy is most often recommended as a treatment option.
- HER2/neu test: HER2/neu protein is found on some types of cancer cells. This test shows whether the tissue has too much HER2/neu protein or too many copies of its gene. If the breast tumor has too much HER2/neu, then targeted therapy may be a treatment option.
Learn more about how hormone status plays a role in breast cancer.
It may take several days to get the results of these tests. These results help your doctor decide which breast cancer treatment options are best for you.
Clinical Breast Exam (CBE) and Breast Self-Exam (BSE)
While the American Cancer Society no longer recommends clinical breast exams or breast self-exams as part of a regular screening schedule, it doesn’t mean they should never be done. Many doctors still perform clinical breast exams on their patients as part of their screening programs. Talk to your doctor to see if this is appropriate for your case. Additionally, most doctors encourage their patients to be aware of any changes they might notice in their breasts and report them immediately.



